Cardiovascular System
The cardiovascular system is composed of the heart, the blood vessels and the blood. It functions as a remarkably efficient transport system. The tissues of the body continuously require nutrients and oxygen and produce waste that requires excretion. Because most cells are only capable of such exchanges with extra-cellular fluid of their immediate environment, a method of renewing that environment is critical in multi-cellular organisms. Cardiovascular system provides for a steady supply of nutrients to the tissues and a removal of waste from the tissues to prevent the toxic pollution of those environments.
I. Blood
The transport medium for the cardiovascular system is the blood. Blood is a connective tissue and is the only fluid tissue of the body. Blood is thicker and more viscous than water and appears relatively homogenous but actually is composed of formed elements including living blood cells suspended in a non- living fluid matrix called plasma. Blood is slightly alkaline and its temperature is typically slightly higher than body temperature. Due to it's high concentration of dissolved ions, it has a slightly saline taste. Blood is opaque and red in color due to the hemoglobin content in erythrocytes (red blood cells). It varies from a bright scarlet color in oxygenated blood to a dull dark red in deoxygenated blood.
Blood volume is regulated and maintained by actions of the several negative feedback systems and the capability of coagulation during trauma to the vascular system. Particularly important is the regulation of water volume involving anti-diuretic hormone aldosterone and atrial natriuretic peptide. This hormones influence the function of the kidney and thus influence the loss of water.
Blood cells include:
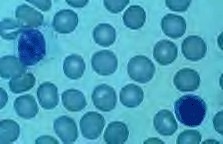
Erythrocytes (Red Blood Cells)
Erythrocytes - contains hemoglobin and transports oxygen and carbon-dioxide
Erythrocytes are relatively small cells with a biconcave shape. Mature erythrocytes do not contain a nucleus. They also do not contain mitochondria, so they produce their energy only through anaerobic processes. They are essentially plasma membranes containing cytosol packed with hemoglobin molecules. Their brief lifespan is due to their lack of a nucleus. Without a nucleus, the normal wear and tear on a plasma membrane and other structures can not be repaired, leading to fragile membranes subject to hemolysis.
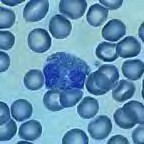
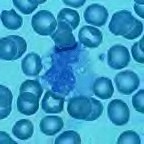
Leukocytes (White Blood Cells)
Leukocytes are mobile cells that move by amoeboid motion. The cardiovascular system serves as a conduit for their circulation, but they have the ability to escape the vessels to enter into the tissues, squeezing through capillary wall fenestrations and process known as diapedesis. Phagocytic leukocytes are attracted to chemicals released by toxins released by microbes, kinins released by damaged tissues, and some of the colony-stimulating factors. These leukocytes travel by amoeboid movement up the chemical gradient towards the source of the chemical release.
Neutrophils - phagocytosis of bacteria; destruction of bacteria through utilization of defensins, lysozyme, or oxidents
Eosinophils - opposes effect of histamine and allergic response and phagocytize antigen-antibody complexes; destroys certain parasitic worms
Basophils - liberates heparin, histamine and serotonin actions to intensify effect
Monocytes - transforms to macrophages; phagocytosis
Lymphocytes - mediate immune response; natural killer cells, B-cells and T-cells
Thrombocytes (Platelets)
Platelets- function in homeostasis; release chemicals to enhance vascular spasm
Platelets are produced by megakaryoblasts that are formed during leukopoiesis. These mature to megakaryocytes, huge cells that burst into fragments of granules encased in plasma membranes.
Platelet plug formation is a component of hemostasis. Platelet plugs typically form in the inner wall in blood vessels in response to trauma. Circulating blood deposits platelets at the injury site that adhere to the collagen fibers uncovered by the damage to the endothelial lining of the vessel. As a result to adhesion, platelets begin to swell and release the contents of their granules, in particular, ADP. ADP increases the "stickiness" of other platelets in the area, causing additional adhesion to the originally activated platelets. This aggregation of platelets reduces blood loss at the point of injury by forming a mass called the platelet plug.
Blood Anatomy
Hemoglobin is carried in the erythrocytes. Each erythrocyte will contain approximately 280 million hemoglobin molecules. A hemoglobin molecule consists of four polypeptide chains, each bound to an iron containing heme group and each heme group will reversibly bind and carry one molecule of oxygen. Hemoglobin carries about 98.5 percent of all the oxygen transported in the cardiovascular system, along with transporting about 23 % of the carbon dioxide that binds to amino acids of the polypeptide chains forming carbaminohemoglobin.
Blood is composed of plasma and formed elements. Centrifuged blood will form an upper layer of plasma (55%), a middle layer called the buffy coat composed of leukocytes and platelets (1%), and a lower layer of erythrocytes (45%) called the hematocrit.
Viscosity of blood is produced primarily as a function of the amount of formed elements in the blood. The greater the ratio form elements to plasma the more viscous the blood becomes.
Hematopoiesis is the production of new blood cells that occurs in the hematopoietic stem cells found distributed in the red bone marrow. Erythropoiesis is the production of new erythrocytes and leukopoiesis is the production of new leukocytes and platelets.
Hemostasis
The extrinsic and intrinsic pathways of blood clotting differ in several aspects. The extrinsic pathways have fewer steps and occurs rapidly. It is triggered by thromboplastin (coagulation factor III) which is released from the surfaces of injured cells and leaks into the blood. Thromboplastin activates clotting factor VII that combines with factor X, thus activating it. Activated factor X combines with factor V to form active prothombinase completing the pathway. The intrinsic pathways is triggered by elements contained within the blood. At damaged or roughened endothelial cells lining the blood vessels, collagen will often be exposed. Adhesion to the collagen by platelets will result in phospholipid release by platelets that activate clotting factor XII. Activated XII will in turn activate factor XI, which activates factor IX. Activating IX will combine with factor VIII and platelet phospholipids to activate factor X. Activated X combines with factor V to form active prothrombinase.
Blood Groups
Erythrocytes contain antigens (agglutinogens) as a component of their plasma membranes. The ABO blood group is based on two antigens A and B which are genetically determined. People whose erythrocytes have only type A antigens are said to have type A blood. Similarly, people with erythrocytes displaying only type B antigens have type B blood. People with erythrocytes displaying A and B antigens have type AB blood, and people with erythrocytes containing no antigens have type O blood. In addition to antigens on the erythrocytes, blood plasma contains antibodies (agglutinins) which react to bind to antigens. An antibody bound to an antigen forms the antigen-antibody complex that will trigger the compliment factors of the blood, resulting in hemolysis of the cell displaying this complex.
- Type A plasma will contain only anti B antibodies that bind to type B antigens.
- Type B blood will only contain anti A antibodies that bind to type A antigens.
- Type AB will contain neither antibodies.
- Type O blood will contain both anti A and anti B antibodies.
In whole blood transfusion care must be taken so donor blood and recipient blood will not form the antigen antibody complex.
People with blood type A blood may receive blood from A or O donors. Type B people are compatible with donors having type B or O blood. Persons with type AB blood may receive blood A,B, AB, or O blood. Type AB is often referred to as the "universal recipient." Those with O type blood are compatible with donor type O only. Type O blood is often referred to as the "universal donor."
During childbirth a small quantity of fetal blood leaks across the placenta to enter the mothers blood stream. If an Rh- mother has given birth to an Rh+ child(inherited from the father), the mothers immune system will respond by producing anti-Rh antibodies that will remain in the blood stream. With a second pregnancy and a fetus carrying the Rh+ gene, and thus Rh antigen, the mother's antibodies can cross the placenta and enter the fetus producing hemolysis of the fetal blood erythrocytes. Rh stands for Rhesus factor, named after the Rhesus monkey from where it was first discovered.
II. Blood Vessels
Blood vessels are of three types: arteries, capillaries, and veins. Arteries convey blood from both ventricles of the heart to virtually every part of the body. They are found in all tissues with the exceptions of the hair, nails, epidermis, cartilage, and cornea. Arteries branch to become smaller vessels, arterioles, which in turn branch to produce capillaries. Capillaries are the ultimate subdivision of the vascular system and it is through the capillaries that the exchange of carbon dioxide, oxygen, water, nutrients, metabolites, and wastes occur between the blood and tissues. Capillaries converge to form the venules, which continue convergence to form the larger veins. Veins serve to return blood to the heart, either from the systemic circuit or from the pulmonary circuit.
The largest artery in the body is the aorta. It receives blood from the left ventricle of the heart. Arteries are more muscular and elastic than the other blood vessels because they receive blood as it is pumped from the heart. Capillaries have thin walls which are composed of only one layer of cells which allows the exchanges to take place between the blood and body tissues. Most veins contain valves, which keep blood from flowing backwards. The two largest veins are the superior vena cava and the inferior vena cava. The superior vena cava brings the blood from the upper part of the body to the right atrium of the heart. The inferior vena cava brings the blood from the lower part of the body also to the right atrium of the heart.
III. Heart
The heart is a four-chambered muscular pump that propels blood through the blood vessels. It is about the size of an adult fist and weighs approximately 300 grams. The heart pumps about 30 times its own weight each minute, 24 hours a day. During activity, the heart's output increases to match the demands of the tissues for oxygen and nutrients. With an average rate of about 70 bpm, a normal heart would pump well over 10 million liters of blood per year.
The heart is located in the mediastinum, extending about 12 cm from the second rib to the fifth intercostal space. It lies anterior to the vertebral column and posterior to the sternum. The heart tips slightly to the left and assumes an oblique position in the thorax and will be partially obscured by the overlapping lungs.
The bulk of the tissue of the heart is the cardiac muscle, or myocardium. It is the activity of this tissue that is responsible for the contractility of the heart. Although similar to striate muscle, it has unique characteristics that provide for its effectiveness and durability.
The right atrium receives blood that returns from the body tissues. The right ventricle receives blood from the right atrium and pumps the blood into the pulmonary artery, which carries the blood to the lungs for oxygenation. The left atrium receives the blood from the lungs and delivers it to the left ventricle which then pumps the blood into the aorta for transportation to the body tissues.
One-way valves in the chambers of the heart keep the blood flowing in the right direction. The tricuspid valve is located between the right atrium and right ventricle. The pulmonary valve is located between the right ventricle and the pulmonary artery. Between the left atrium and the left ventricle is the mitral valve which prevents blood from flowing back into the left atrium once it is delivered to the left ventricle. The aortic valve is located between the left ventricle and the aorta.
Blood Pressure
The muscles of the heart work together in a cyclic manner. First, the atria contract and force blood into the ventricles. The atria relax and blood returning from the body and lungs enter into the atria. As the atria are filling, systole begins, and the ventricles contract. Thus, the period of ventricular rest is known as diastole and the ventricular contraction period is called systole. The pressure is much greater in the arteries during contraction as blood is forced through the vessels and is lower during the period of rest.
Conduction
Electrical impulses originate in the heart from groups of nerve cells called "pacemakers" and spread throughout the muscles causing cyclic contractions. The sinoatrial (SA) nodecauses the right atrium to contract. The atrioventricular (AV) node sends electrical impulses through the bundle of His, nerve fibers in the septum. The bundle of His divides into a right bundle branch and a left bundle branch. The bundle branches further divide into the Purkinje fibers, a network of nerve fibers throughout the ventricles causing all the muscles of both ventricles to contract. It takes about 0.8 seconds for this electrical conduction pattern to occur.
Review Questions:
1. Describe what blood is composed of.
2. What are the functions of RBC's?
3. What are the functions of WBC's?
4. What are the functions of platelets?
5. Why is AB blood called the universal recipient?
6. Why is O blood called the universal donor?
7. Outline the flow of blood from the heart and back. Name the part of the heart blood leaves from and returns to, and name the blood vessels that take blood away and return it to the heart. Trace blood through the different types of blood vessels and indicate in which vessels exchanges take place between blood and body tissues.
8. Name the chambers of the heart and describe what their function is.
9. Describe the events of a single cardiac cycle.
10. What two chemicals directly affect the activation of the heart and what are their roles?